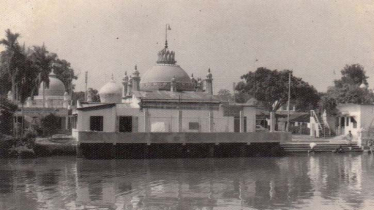
Photo : Messenger
Mpox is an illness caused by the monkeypox virus. It is a viral infection which can spread between people, mainly through close contact, and occasionally from the environment to people via things and surfaces that have been touched by a person with mpox. In settings where the monkeypox virus is present among some wild animals, it can also be transmitted from infected animals to people who have contact with them. Following a series of consultations with global experts, WHO has begun using a new preferred term, "mpox,” as a synonym for monkeypox.
Mpox can cause a range of signs and symptoms. While some people have less severe symptoms, others may develop more serious illnesses and need care in a health facility. Common symptoms of mpox include a rash, which may last for 2–4 weeks. This may start with, or be followed by, fever, headache, muscle aches, back pain, low energy and swollen glands (lymph nodes). The rash looks like blisters or sores, and can affect the face, palms of the hands, soles of the feet, groin, genital and/or anal regions. These lesions may also be found in the mouth, throat, anus, rectum, or vagina, or on the eyes. The number of sores can range from one to several thousand. Some people develop inflammation inside the rectum (proctitis) that can cause severe pain, as well as inflammation of the genitals that may cause difficulties urinating.
In most cases, the symptoms of mpox go away on their own within a few weeks with supportive care, such as medication for pain or fever. However, in some people, the illness can be severe or lead to complications and even death. Newborn babies, children, people who are pregnant and people with underlying immune deficiencies, such as from advanced HIV disease, may be at higher risk of more serious mpox disease and death.
Severe disease due to mpox may include larger, more widespread lesions (especially in the mouth, eyes and genitals), secondary bacterial infections of the skin or blood, and lung infections. Complications can include severe bacterial infection from skin lesions, mpox affecting the brain (encephalitis), heart (myocarditis) or lungs (pneumonia), and eye problems. People with severe mpox may require hospitalisation, supportive care and antiviral medicines to reduce the severity of lesions and shorten time to recovery.
According to available data, between 0.1% and 10% of people with mpox have died. It is important to note that death rates in different settings may differ due to several factors, such as access to health care and underlying immunosuppression, including because of undiagnosed HIV or advanced HIV disease. Mpox spreads from person to person mainly through close contact with someone who has mpox. Close contact includes skin-to-skin (such as touching or sex) and mouth-to-mouth, or mouth-to-skin contact (such as kissing), and can also include being face-to-face with someone who has mpox (such as talking or breathing close to one another, which can generate infectious respiratory particles). During the global outbreak that began in 2022, the virus mostly spread through sexual contact. More research is needed on how mpox spreads during outbreaks in different settings and under different conditions.
People with mpox are considered infectious until all their lesions have crusted over, the scabs have fallen off and a new layer of skin has formed underneath, and all the lesions on the eyes and in the body (in the mouth, throat, eyes, vagina and anus) have healed too, which usually takes from 2 to 4 weeks.
It is also possible for the virus to persist for some time on clothing, bedding, towels, objects, electronics and surfaces that have been touched by a person with mpox. Someone else who touches these items may become infected, particularly if they have any cuts or abrasions or touch their eyes, nose, mouth, or other mucous membranes without first washing their hands. Cleaning and disinfecting surfaces/objects and cleaning your hands after touching surfaces/objects that may be contaminated can help prevent this type of transmission.
The virus can also spread during pregnancy to the fetus, during or after birth through skin-to-skin contact, or from a parent with mpox to an infant or child during close contact.
Although getting mpox from someone who is asymptomatic (not showing symptoms) has been reported, there is still limited information on whether the virus can be transmitted from someone with the virus before they get symptoms or after their lesions have healed. Although live virus has been isolated from semen, we do not yet know the extent to which infection can spread through semen, vaginal fluids, amniotic fluids, breastmilk, or blood.
From animals to humans:
Someone who comes into physical contact with an animal which carries the virus, such as some species of monkeys or a terrestrial rodent (such as the tree squirrel), may also develop mpox. Exposure by such physical contact with an animal or meat can occur through bites or scratches, or during activities such as hunting, skinning, trapping, or preparing a meal. The virus can also be caught through eating contaminated meat which is not cooked thoroughly.
The risk of getting mpox from animals can be reduced by avoiding unprotected contact with wild animals, especially those that are sick or dead (including their meat and blood). In countries where animals carry the virus, any food containing animal parts or meat should be cooked thoroughly before eating.
From humans to animals:
There have been a few reports of the virus being identified in pet dogs. However, it has not been confirmed whether these were true infections or whether the detection of virus was related to surface contamination. Since many species of animals are known to be susceptible to the virus, there is the potential for spillback of the virus from humans to animals in different settings. People who have confirmed or suspected mpox should avoid close physical contact with animals, including pets (such as cats, dogs, hamsters, gerbils), livestock and wildlife.
People who have close contact with someone who has mpox are at risk of infection. Close contact includes skin-to-skin (such as touching or sex) and mouth-to-mouth, or mouth-to-skin contact (such as kissing), and can also include being face-to-face with someone who has mpox (such as talking or breathing close to one another, which can generate infectious respiratory particles). People who have contact with clothing, bedding, towels, objects, electronics and other surfaces that have been touched by someone with mpox are also at risk.
Anyone living with someone who has mpox should take steps to reduce the risk of becoming infected. A person who has been diagnosed with mpox should be assessed by a health care provider to determine if they are well enough to be cared for at home and if isolation can be safely managed at home. Health workers should follow infection prevention and control measures to protect themselves while caring for patients with mpox. To protect yourself and others against mpox, know the signs and symptoms, how the virus spreads, what to do if you get ill, and the risk in your area or community.
If the virus is spreading in your area or in your community, have open conversations with those you come into close contact with about any symptoms you or they may have. Avoid close contact with anyone who has mpox, including sexual contact. Clean your hands frequently with soap and water or an alcohol-based hand rub.
If you think you might have mpox, you can act to protect others by seeking medical advice and isolating from others until you have been evaluated and tested. If you have mpox, you should isolate yourself from others until all your lesions have crusted over, the scabs have fallen off and a new layer of skin has formed underneath. This will stop you from passing on the virus to others. Follow your local health authority instructions on isolation at home or in a health facility. If having sex, use condoms as a precaution for 12 weeks (about 3 months) after you have recovered.
In countries where some animals have been found to carry the monkeypox virus (i.e. some countries in in east, central and west Africa), protect yourself by avoiding unprotected contact with wild animals, especially those that are sick or dead (including their meat and blood). Any food containing animal parts or meat should be cooked thoroughly before eating.
Contracting mpox during pregnancy (which is considered a relative immunosuppressed state) can be dangerous for the fetus or newborn infant and can lead to loss of the pregnancy, stillbirth, death of the newborn, or complications for the parent. If you are pregnant, avoid close contact with anyone who has mpox. Anyone who has close contact with someone who is infectious can get mpox, regardless of who they are. If you think you have been exposed to or are showing symptoms that could be mpox, contact your healthcare provider. They will help you get tested and access the care you need.
The writer is a Health Research Worker and Health Activist. He can be reached at: [email protected].
Messenger/Fameema